BCV is the only therapeutic ventilation intervention that supports both inspiratory and expiratory work of breathing in a physiologically natural way, providing a real alternative to positive pressure techniques while avoiding most side effects. BCV allows patients to eat, speak and drink while their breathing is fully supported.

BCV is a real non-invasive ventilator without the harmful side effects of mask or PPV. Advantages include safe lung recruitment, volume expansion, improved gas exchange, and multifunction capabilities, such as HFCWO and cough options.
BCV delivers multifunction capabilities with a single interface, a cuirass shell. It decreases the use of sedation, decreases the overall risk of hospital-acquired infections, and reduces patients’ length of stay. BCV is a significant cost saving tool for treating cardiopulmonary patients, available for both hospital and home.
Ventilation with active exhalation means Hayek BCV is particularly efficient for CO2 clearance. The non-mask cuirass interface allows avoidance of the side effects typically associated with facial mask or invasive positive pressure ventilation.

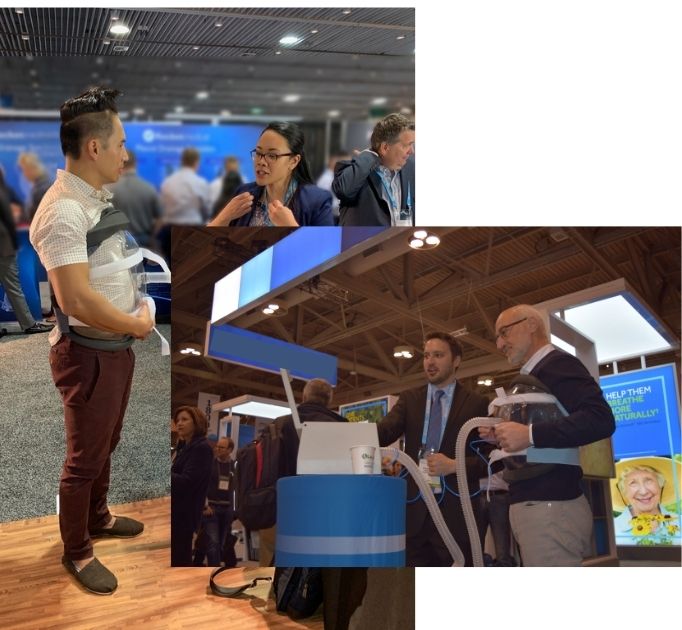
Learn why these medical professionals strongly believe in BCV, and let them explain the value it can bring Hospitals, ICUs, LTACHs and Home Care patients.
BCV can help manage the symptoms associated with many conditions affecting the lungs, including but not limited to ALS, COPD, ARDS And Many More!
